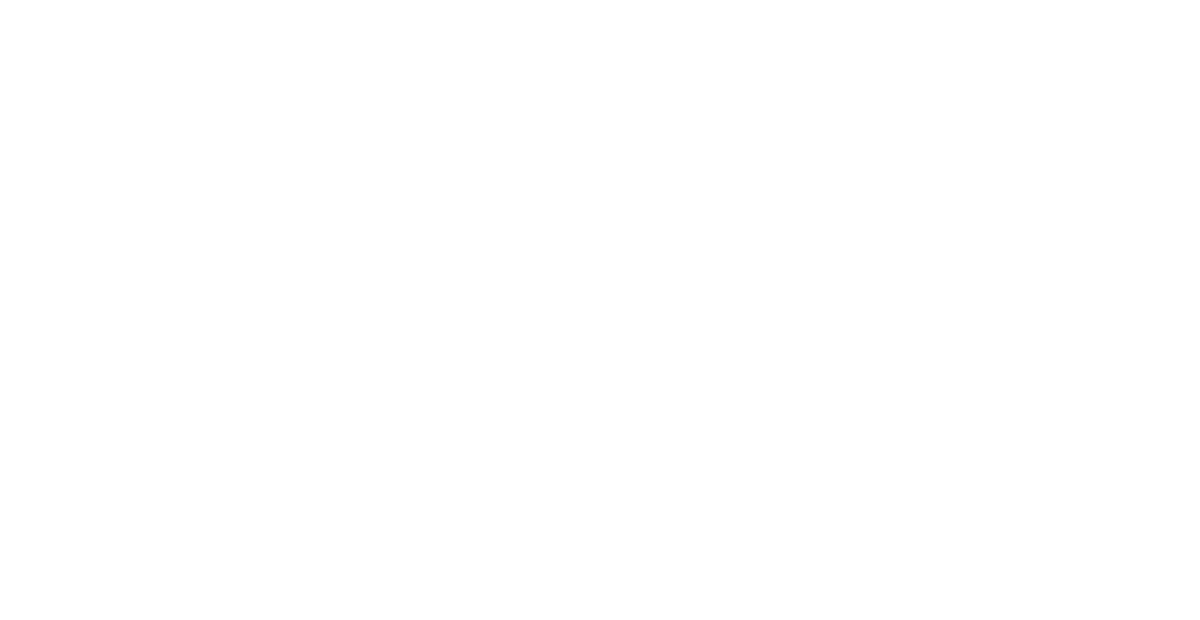
Percutaneous Transluminal Coronary Angioplasty (PTCA)
AORTA
Transport Oxygenated
blood to the body
CORONARY ARTERIES
Blood supply to the heart
It has been recommended that you undergo coronary angioplasty to treat one or more blockages in the coronary arteries which are the arteries that supply the blood and oxygen to the heart muscle. Your coronary angiogram identified the location and the extent of the blockage/s and after review of the angiogram it was thought that angioplasty was the best treatment option. The two other options for treating the narrowing would include medical treatment and coronary artery bypass surgery. If you have any questions regarding the selection of the type of treatment in your situation, please discuss this with your Cardiologist.
It is very important that you take Aspirin and Clopidogrel the day of the PTCA and all other medication as directed by your Doctor. Any questions should be asked of your Cardiologist before the procedure.
The Angioplasty Procedure
The angioplasty procedure in a number of ways is quite similar to the diagnostic coronary angiogram that you have already undergone.
The procedure is done in the Cardiac Catheterisation Laboratory. You will be given sedation before and during the procedure. It is very important that you take Aspirin and Clopidogrel the day of the PTCA and all other medication as directed by your Doctor. Any questions should be asked of your Cardiologist before the procedure.
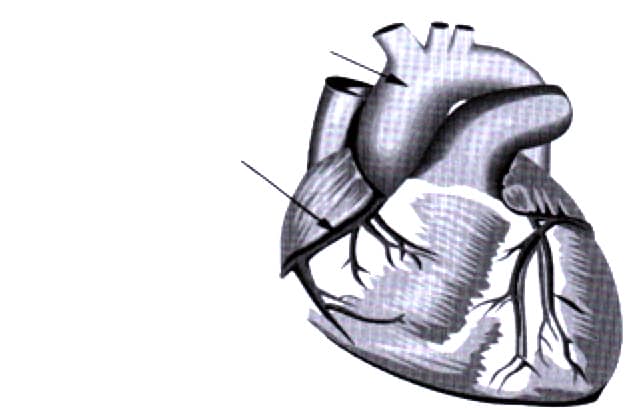
The initial part of the procedure involves placing a short plastic tube (sheath) into the femoral artery in the groin after using local anaesthetic to anaesthetize the area. Local anaesthetic is injected with a small needle. Sometimes other sites, the left groin or the right or left radial or brachial arteries at the wrist and elbow respectively are used to provide an access port and allow us to reach the heart and perform the angioplasty. Once access into your artery has been obtained by placement of sheath a special tube called a guiding catheter, which is similar to the angiography catheters, is passed up to your heart.
Generally, this is a painless procedure and you are not aware of any sensation during the passage of this catheter from the access site in your groin up to your heart. Once the catheter reaches the heart it is placed into the mouth of the appropriate coronary artery where the blockage is and several angiogram pictures are taken to use as “road maps” during the procedure. The next step is to pass a very fine guide wire down through the guiding catheter into the artery through the blockage and into the distal or downstream artery.
Insertion of introducer Sheath into the femoral artery
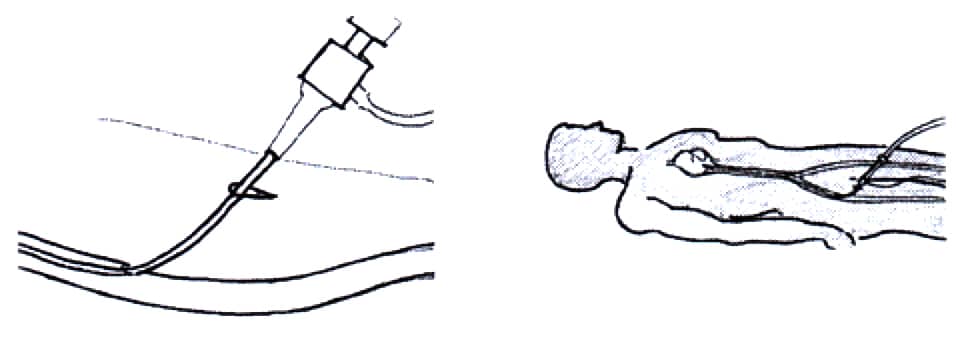
This wire then serves as a “railway track” if you like and allows us to pass the catheter to enlarge the blockage. This catheter has on the end of it a small inflatable balloon that will stretch open the blockage and then be deflated and removed from the artery. Following the initial opening of the artery, repeat angiograms are taken to assess the result of the initial treatment. Usually a stent is then placed into the blockage.
Balloon inflation in a coronary artery
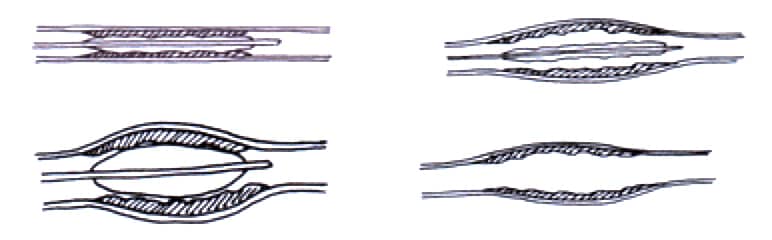
This stent device is a stainless-steel mesh device which is manufactured and mounted in the factory onto an angioplasty balloon catheter. This device is then positioned into the blockage in your artery using the x-ray guidance and the balloon is inflated. This expands the wire mesh which then stays expanded after removal of the balloon and scaffolds open the artery. Where appropriate a special drug coated stent will be used. The drug coating helps to reduce the chance the treated blockage will recur. The placement of the stent has several advantages; it usually results in a larger opening and therefore produces a better short term result; it may also make the artery less likely to collapse shut after the procedure; and it also appears to reduce the chances that the blockages will return in the future. Once the stent is deployed successfully repeat angiograms are taken to confirm a satisfactory result.
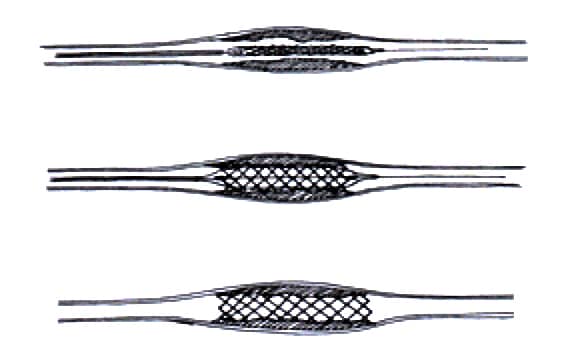
Stent placement in a coronary artery
Post Procedure
Once the procedure is completed you will be transferred back to the angioplasty unit or Coronary Care Unit with the small sheath still in place in your groin. This will be removed once the intravenous Heparin (blood thinner) wears off so the blood will clot when the tube is removed. The sheath is then removed, and pressure is applied to the artery until it seals itself.
You will then be kept in bed for a number of hours after the procedure and usually overnight until the following morning. Often these days a small plug or suture will be placed into the artery to seal it before you leave the Catheterisation Lab. If this is done, you will be able to sit up and to mobilise much sooner following the procedure.
Routinely, before the angioplasty you will be given Aspirin and a medication called Clopidogrel to interfere with the action of the platelets in the blood which are involved in blood clotting. These drugs reduce the risk that the artery will occlude during or shortly after the procedure. In addition, you will be given intravenous Heparin which also serves to prevent blood clotting during and shortly after the procedure. On some occasions we will also use a medication called Reopro which also affects the platelets more effectively then Aspirin and Clopidogrel and is given by an infusion during the procedure. This also reduces the risk of blood clot formation in the artery and is used in selected circumstances.
Angioplasty is generally a very successful procedure to treat a stenosis in a coronary artery. Success rates without any major complications in excess of 95% should be expected. As with any medical procedure there is the risk of possible complications associated with the angioplasty of your coronary arteries. Occasionally after treatment of the blockage, the blockage will recoil and cause acute closure of the artery. This can potentially cause an acute heart attack if it is not treated quickly and successfully. Fortunately, the development of intra-coronary stents has meant that usually this type of vessel closure can be treated successfully. If not, it may result in myocardial infarction or heart attack and also possibly the need for an emergency coronary artery bypass graft operation performed immediately upon transfer from the Catheterisation Laboratory to the Cardiac Operating Theatre. The risk of a heart attack is perhaps 1 or 2 changes in every 100 angioplasties.
The risk of needing an emergency CABG operation is less than 1 chance in 300 PTCA procedures. In addition, there is the very small risk perhaps 1:1000 of death occurring as a result of these complications or some other catastrophe. A number of the risks are similar to those of the coronary angiogram and they include the risks of a stroke or an allergic reaction to the x-ray dye which can occur in perhaps 1in 20,000 patients. This is obviously a very rare complication because during angioplasty blood thinners such as Heparin, Aspirin, Clopidogrel and Reopro are used there is the risk that these medications can induce bleeding. Bleeding is common from the access site at the femoral artery in the groin but could be from anywhere including the gut or even an intra-cranial haemorrhage. The risk of significant groin complication is perhaps 2-3 chances in 100. The risk of a cerebral haemorrhage is very rare and there is less than one chance in 1000 that this might occur. Again, in a similar way to coronary angiography, it is possible to damage the access artery during the angioplasty. Usually this simply results in a significant bruise or haematoma but occasionally can result in an AV fistula or a pseudo aneurysm of the artery. Occasionally, the plug can cause occlusion of the access artery. These vascular complications may require surgical treatment. The greatest risk of complications during the angioplasty is at the time of the procedure in the Catheterisation Laboratory. Sometimes, the artery can recoil or collapse in the first 12 – 24 hours after the procedure and this is why you are going to be kept in Hospital after the procedure.
Following Hospital discharge there is a very small risk, perhaps one in a hundred, that if you have received a stent this could suddenly occlude with a blood clot and produce an acute heart attack.
Therefore, if you develop serious chest pain you should present immediately to the Hospital. Taking Aspirin and Clopidogrel for at least 12 months after the procedure will substantially reduce the chance that this may occur.
Perhaps the long-term complication of greatest concern is the chance that the blockage that has been successfully treated will re-narrow again and begin to cause angina yet again. Usually if the artery is going to re-narrow it occurs between the fourth and tenth month after the procedure. If all is well at 12 months, it is unlikely that the blockage that has been treated with angioplasty will again cause problems. The re-narrowing that can occur is the result of ingrowth or scar tissue at the site of the original blockage causing a new blockage made up of this soft scar tissue. The new drug coated stents reduce the risk of re-narrowing substantially. If re-narrowing occurs it can be treated by repeat PTCA using a balloon catheter and a further stent can be deployed. Sometimes a coronary bypass operation is needed.
Having read this information sheet about coronary angioplasty please feel free to ask your Cardiologist for clarification of any further points or ask any other questions you would like prior to the procedure.
Discharge Information
- You will be unable to drive a vehicle for 48 hours following your angioplasty (National Road Transport Commission regulations).
- For 48 hours splint or apply pressure to the puncture site when sneezing or coughing (if your angioplasty was performed through the groin).
- Observe your puncture site for the next week following your angioplasty. You may expect some bruising to develop.
- Remove the plastic dressing covering your puncture site 48 hours after the angioplasty.
- If you have increasing pain, redness or signs of infection, swelling or fluid oozing from the puncture site, please see your GP or call our rooms.
- Bleeding rarely occurs at the puncture site once you have been discharged from Hospital. If it does occur, apply firm pressure for 10 to 15 minutes or until the bleeding stops and seek medical assistance by phoning or see your GP or call our rooms. If there is a lot of bleeding call an Ambulance.
- You should not experience any weakness or altered sensation in the limb (leg or arm) nearest the puncture site. If you do, see your GP or call our rooms.
- It is recommended that you do not lift heavy objects (>10kgs) for at least 5 to 7 days. Strenuous exercise and activities should be avoided within the first week. Activities and exercise routines should be increased over a fortnight to normal levels.
- Normal physical activity such as walking and general movement without placing any stress on the wound area is fine.
- If you develop any chest pain or discomfort after the angioplasty it is important that you inform your GP or Cardiologist as soon as possible.
- It is very important that you take your medications as prescribed by your Doctor. Taking Aspirin daily and Clopidogrel (Iscover or Plavix) 75mg per day together are important following your angioplasty. These medications work in conjunction to prevent blood cells (platelets) clumping together and forming a clot inside the artery which has been stented.
- Commencing a cardiac rehabilitation program is strongly encouraged. This will help most patients reduce their risk of further coronary heart disease, while offering useful information about lifestyle, medication and exercise management. A cardiac rehabilitation Nurse will visit you in Hospital prior to discharge.
- Contact our rooms on 07 4779 0199 for advice.




 Referrals & Patient Enquiries:
Referrals & Patient Enquiries: